Employee Benefits Market Check Survey: Affordability & Alternative Provider Networks
Healthcare costs continue to rise, placing significant pressure on employers and employees. The 2025 renewal cycle was the most challenging in the last four years, and companies will need to explore more aggressive strategies to make an impact.
On March 20, we conducted a survey to gain insight into whether employers believe benefits affordability is a challenge for their workforce. We also sought to understand if employers will explore different provider networks to combat the escalating costs. The results are in the charts below.
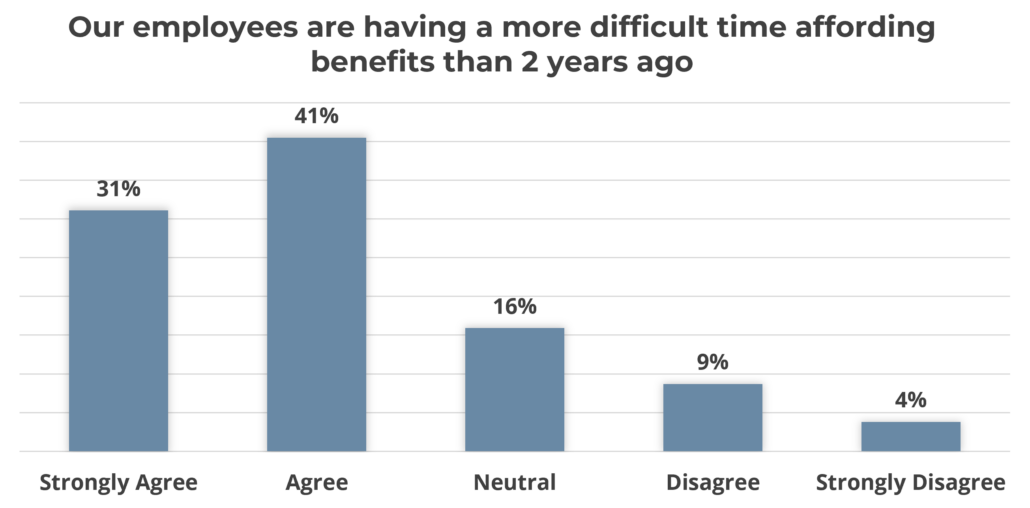
*Results based on 264 employer respondents.
We asked the same question of employers in 2022, and 47% of respondents agreed/strongly agreed that employees were having a more difficult time affording their benefits. In three years, that has increased to 72%. Employers and employees may find themselves at a crossroads very soon.
Alternative Provider Network Options
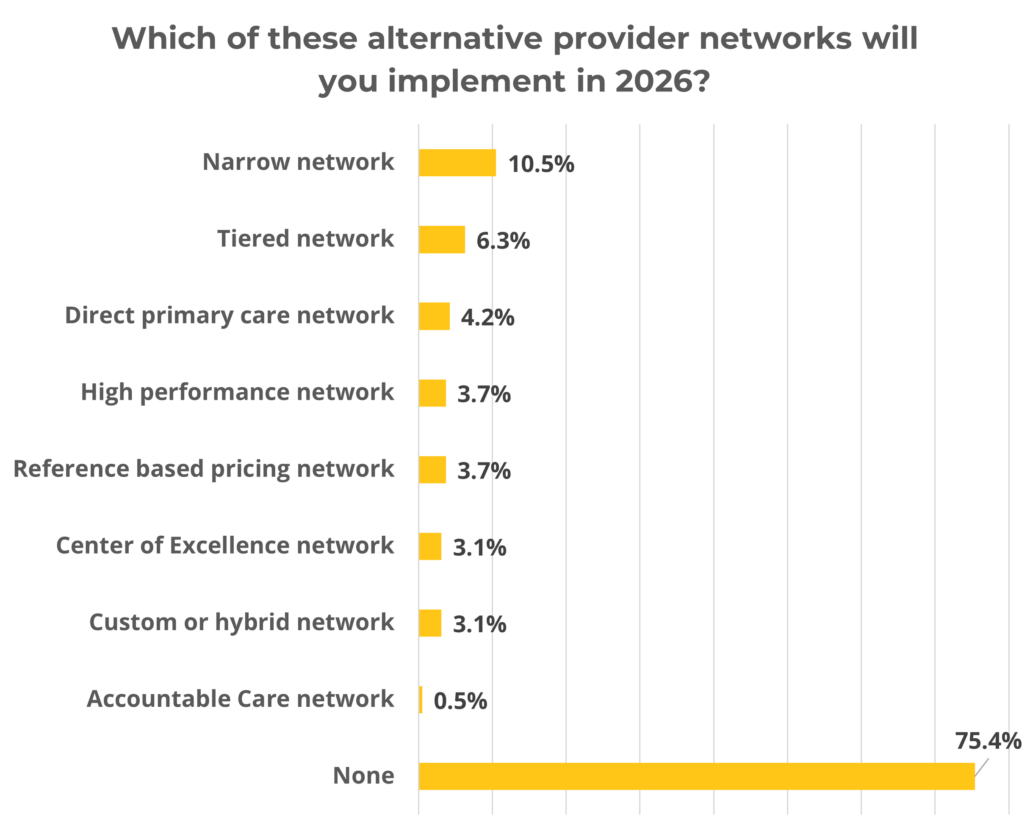
Key Findings
The January 2025 renewal cycle was difficult, with 39% of employers seeing their medical costs increase by 7% or more after all changes were implemented. Further, 34% of employers changed payroll contribution amounts, and 19% changed plan design. When these changes occur, they have a direct impact on the plan’s affordability for the employee. Business leaders must explore other options that can improve quality and affordability.
One lever employers can pull, which will not impact a worker’s paycheck, is adjusting the type of provider network offered to the workforce. The traditional network provides access to almost all providers with discounted fees. While access is rarely an issue, these networks typically do not differentiate between cost, quality, or outcomes. Given the complexity of change and the need to balance disruption with cost control, it’s not surprising that most employers aren’t implementing an alternative network. However, with rising costs, now may be the time to evaluate whether narrowing networks or directing employees to the providers that can offer care at the very best level can help plan sponsors manage healthcare trends without asking employees to shoulder more of the financial burden.
Should you have any questions regarding any of this information or want to discuss affordability, network options, or industry-level data, please contact your local Assurex Global adviser.
Alternative Network Definitions
Narrow Network – limits coverage to smaller group of providers; employees have less choice but receive savings.
Tiered network – categorize providers into tiers based on quality and cost; employees pay less (lower copays/deductibles) when choosing providers in higher tiers
High-performance network – includes providers that meet high standards for cost, efficiency and outcomes
Direct primary care network – employer contracts directly with providers for unlimited access; employees pay a flat fee
Center of Excellence network – specific procedures are done at specialized hospitals or clinics; employees receive high-quality care but may need to travel
Accountable Care Organization network – Groups of providers who coordinate care to improve quality and are incentivized via a shared savings program
Reference Based Pricing network – sets fixed provider reimbursement rate based on Medicare or similar; employees pay more if cost is above reference rate
Hybrid/Custom network – A combination of elements from other models above.




Leave a Reply
Want to join the discussion?Feel free to contribute!