Employee Benefits Market Check Survey: Transparency Disclosure Requirements
Transparency in healthcare costs has been elusive in the U.S. There have been prior attempts to help consumers understand how much they will spend for a given procedure without much success. The federal government is again trying to help in this effort. In 2020, the government passed the transparency in coverage (TiC) regulations. The TiC rules require group health plans and insurers to make two machine-readable files available on a public website. These files contain detailed pricing data for all covered services. One file contains in-network negotiated rates, and the other includes out-of-network allowed amounts.
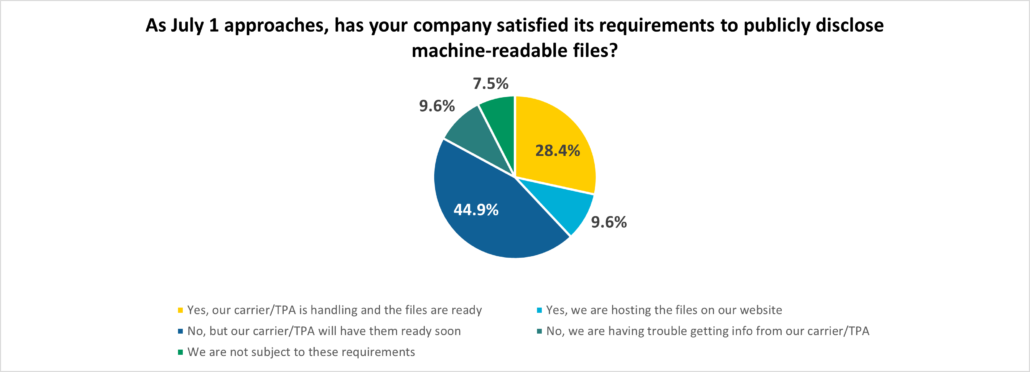
We conducted a poll during a webcast on June 23 to gain insight into whether employers will meet their requirements. The results are in the chart below.
Key Findings
The encouraging part of the data is that less than 10% of employers required to disclose are having difficulty doing so. The vast majority are ready or will be in short order. For those in the minority, it is imperative to check with your administrator to learn when the files will be ready, or you may need to change vendors. As fiduciaries, employers are responsible for ensuring the files are accessible.
Should you have any questions regarding any of this information, please contact your local Assurex Global adviser.




Leave a Reply
Want to join the discussion?Feel free to contribute!